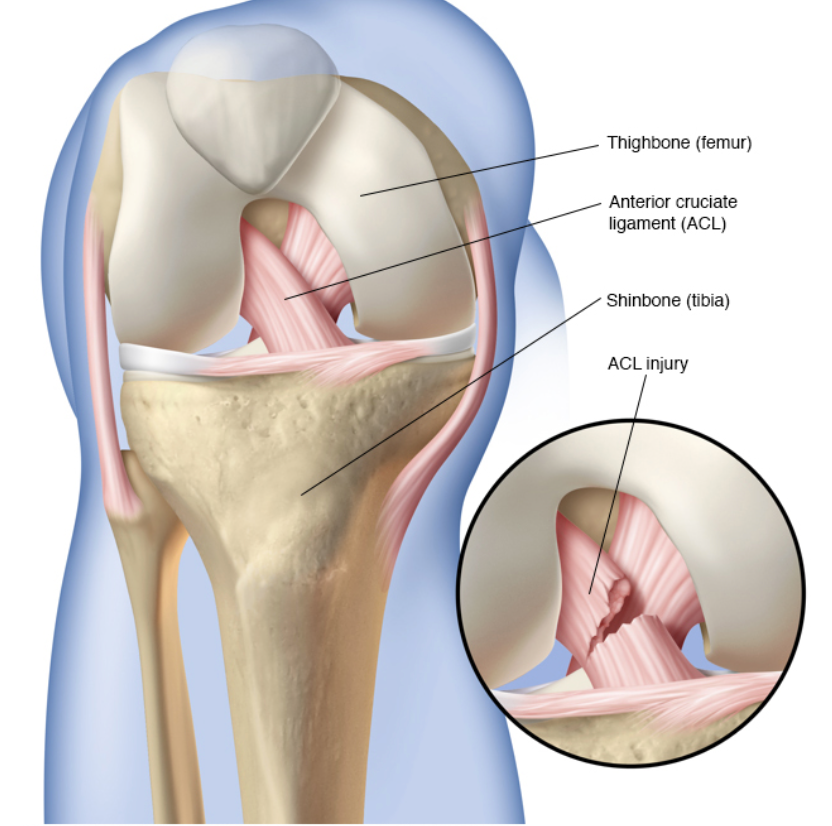
Anterior Cruciate Ligament Injuries (ACL)
One of the most common sporting injuries sustained to the knee. This ligament is one of the key stabilisers of the knee and provides rotational stability to the knee. This injury is commonly sustained when your foot is stationary on the ground and the body rotates around it, producing a pivoting and rotating force at the knee. Such an external rotatory force tears the anterior cruciate ligament, and 50% of these are associated with injuries to the cushioning cartilage of the knee (meniscus).
At the time of injury, patients often feel a snapping sensation followed by immediate swelling of the knee over the first 24-hour period. It is difficult to examine a painful swollen knee, hence medical practitioners may not be able to ascertain the nature of injury immediately. However, it is advised to see an emergency physician to ensure that there are no associated fractures, this is done by obtaining an x-ray. Radiographs may sometimes suggest an ACL injury.
If there is no bony injury the best treatment option is to rest it in a splint and then apply cold packs to reduce the chances of bleeding inside the knee.
The swelling and discomfort will gradually ease and by the end of two weeks, movements of the knee will become less painful and improved. This is the best time to re-assess the knee and examine for ligamentous laxity.
A high index of suspicion can be made based on the mechanism of injury and clinical examination findings. If so, this should be confirmed with an MRI scan.
Management of an ACL injury
Isolated ACL injuries can be managed either non-surgically or surgically. There are no absolute indicators for reconstructing an ACL tear. With young patients, particularly those involved in rotational prone sports, where they are likely to do more damage to their knee with ongoing instability thereby injuring remaining cartilage and ligaments, it is mandatory that these patients have their ACL reconstructed.
If you are not involved in sporting activity or if your knee does not feel unstable, then non- operative management, including physiotherapy, will focus on rehabilitation and promoting appropriate muscular stability at the knee joint.
If you have torn your ACL, and your knee is unstable and you wish to remain active, it is best managed with an ACL reconstruction.
When should the ACL be reconstructed?
Timing of ACL reconstruction is dependent on the associated injuries. If there is a tear in the meniscus or damage to the chondral surface with a bone/cartilage fracture, then more urgent surgery is beneficial for repairing the bone/cartilage defect. An isolated ACL injury should never be acutely repaired because the swelling and inflammation in the joint capsule can make the knee go stiff post-surgery. Therefore, these patients should wait at least three months before reconstructive surgery. A longer wait is not harmful, as long as you are careful with your activities to ensure no further damage.
What happens with an ACL reconstruction?
The reconstruction is performed through keyhole surgery in the knee. An additional cut is made on the inside aspect of the knee to remove the graft. The common graft used is the hamstrings tendon (two of them) from the inside of the thigh. These are then doubled and inserted through drill holes in the leg and thighbone to replace the original ACL ligament. They are fixed to the bone by screws and buttons. Alternate graft options include the patellar tendon from the front of the knee
Patients are allowed to weight bear as tolerated with crutches and discharged home with advice for physiotherapy. Crutches are required for 4 to 6 weeks post-surgery, then patients are allowed a graduated exercise program to improve their function and strength. Contact sports should be avoided for the following 12 months.
With the ACL being a unique ligament complex, it is extremely difficult to recreate the exact anatomy, this means the strength of the reconstructed ligament is never as good as the original ligament.
The potential complications of this surgery include:
- Infection (Very low)
- Stiffness
- Progressive instability
- Numbness in front of the knee.