Bunions
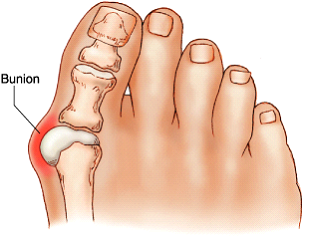 The most common foot complaint treated by an orthopaedic surgeon is a Bunion. (medically known as Hallux Valgus). The term “hallux valgus” is Latin and means a turning outward (valgus) of the big toe (hallux). The bone, which joins the big toe, (the first metatarsal) becomes prominent on the inner border of the foot. This bump is the bunion and is made up of bone and soft tissue.
The most common foot complaint treated by an orthopaedic surgeon is a Bunion. (medically known as Hallux Valgus). The term “hallux valgus” is Latin and means a turning outward (valgus) of the big toe (hallux). The bone, which joins the big toe, (the first metatarsal) becomes prominent on the inner border of the foot. This bump is the bunion and is made up of bone and soft tissue.
Most patients ask, how is the bunion is caused? An exact cause is difficult to predict. By and large the most common cause is ill-fitting shoes, which deviate the toes because of lack of room to accommodate in front of the shoes. Studies have shown that 85% of women wear shoes that are too small for their size and of these 55% develop bunion deformity. Small percentages are hereditary. Other causes of this deformity are neurological, such as cerebral palsy, polio and arthritis.
Bunion deformity can become painful as it progresses, causing pressure and irritation in shoes. Wearing appropriate shoes, which do not allow the toe deformity to progress, therefore can help prevent pain. Not all bunion deformities require surgical correction, as they are not painful. Non-painful bunions should not be operated on as these may become painful post-surgery. It is important to note that these surgeries are not cosmetic surgery and should only be done for pain relief and mechanical problems.
The best investment for foot problems is good footwear. Always wear well-fitting shoes, which match to your foot shape and are comfortable to walk in.
Tips for good shoes:
- Do not select shoes by the size marked inside the shoe. Sizes vary among shoe brands and styles. Judge the shoe by how it fits on your foot.
- Select a shoe that conforms as nearly as possible to the natural shape of your foot.
- Have your feet measured regularly. The sizes of your feet change, as you grow older.
- Have both feet measured. Most people have one foot larger than the other. Fit to the largest foot.
- Fit at the end of the day when your feet are the largest.
- Stand during the fitting process and check that there is adequate space (3/8″ to 1/2″) for your longest toe at the end of each shoe.
- Do not expect shoes to stretch as you walk on it.
- It is a misnomer that fashionable shoes are uncomfortable. They can be made comfortable with the correct fit.

When and why surgery is required
When good shoes, the use of inserts or fillers, do not provide the required pain relief or if there is progression of deformity causing pressure inflammation in the area of the foot, surgical correction may be necessary.
What is involved in bunion surgery?

Surgical correction is offered if the surgeon is convinced that it can improve pain and function with minimal risks. Main risk factors, which can compromise the foot surgery, include diabetes mellitus, poor blood circulation to the foot, and smoking.
Most common surgery offered is correction of the big toe and associated lesser to deformity.
The first long bone (first metatarsal) is cut, realigned and fixed with screws. The second toe bone is cut and realigned and fixed with screws. The soft tissues around the first toe is resected and re-tensioned to retain the bony correction.

Before Surgery


After Surgery



Other surgical options available for this problem include:
- Fusion of the big toe (if there is severe arthritis associated with the deformity).
- Excision of the first toe joint.
- Removal of the bump without any correction. (Poor outcome because of high recurrence rate.)
Foot surgery is associated with risks and complications. As mentioned earlier diabetes and smoking increase the risk of wound infection and non-healing of the bone. Patient satisfaction in foot surgery is around 70% – 80%. The degree of a patient’s pain and deformity determines the satisfaction level.
Main complications that can arise from bunion surgery include:
- Recurrence
- Infection and wound breakdown
- Stiffness and progressive arthritis
- Numbness around the toe
- Painful neuroma (Nerve scarring)
- Scar thickening (Keloid) and associated pain
What to expect after a bunion surgery?
You will have an overnight stay in hospital. In general, there would be no plaster applied to your foot, instead you will have a bulky dressing. You will be fitted with a boot with Velcro strapping and a rigid sole to prevent any damage to the corrective surgery made to your foot. You are allowed to walk on it. Mr. Unni will make arrangements for this to be fitted while you are in hospital and therefore can start walking on your foot the very next day after surgery.
Post-surgery, you may put weight on your foot as much as you can tolerate. Walking long distances is not advisable. When you are not walking, it is advisable to elevate your foot to reduce the swelling. You may require a walking stick or frame depending on your level of comfort, this will be advised by the physiotherapist while you are in hospital.
You will be seen by the orthotist at 3 weeks for a wound check and fitting of the shoes. Mr. Unni will perform a clinical assessment 6 weeks post-operation. Following this you will be sent to a physiotherapist for stretching exercises. It is important that you wear a compression bandage or stockings throughout the post-operative period for a minimum of 3 months. This is to reduce the swelling, aid recovery and improve the function.
Normal footwear can be worn at 6-8 weeks.
It is best to avoid high heels for a minimum of 6 months post-surgery.
