Osteoarthritis of the Hip
Osteoarthritis is one of the most common causes of hip pain in patients. It may be primarily due to inflammation, poor blood supply to the head of the femur or previous injury. Management of this condition involves both non-operative treatments and operative treatment options.
Non-operative treatments involve:
- Analgesia
- NSAID’s (non-steroidal anti-inflammatory medication)
- Physiotherapy
a. regular exercise like swimming, water aerobics or cycling to keep your joint functioning and improve strength and range of motion.
b. directed physiotherapy strengthening program. - Weight loss
a. If you are overweight it is absolutely necessary to lose weight. A BMI over 30 is reported to have a poor recovery outcome in any joint surgery. - Activity modification
Operative treatments involve:
Operative management of this problem involves hemiarthroplasty (replacement of half the hip joint) or total hip replacement (full replacement of the hip joint).
Commonly, the first symptom of osteoarthritis of the hip may appear as discomfort and/or stiffness in your groin, buttock, or thigh when you wake up in the morning. The pain flares up with activity and gets better with rest.
Without treatment for hip osteoarthritis, the condition naturally continues to worsen until rest no longer relieves the pain. The hip joint becomes stiff and inflamed. Bone spurs can build up at the edges of the joint with bones rubbing directly against each other and causing the cartilage to wear down. This makes movement of the hip very painful and may cause an inability to rotate or bend your leg at the hip. If you become less active to avoid the pain, the muscles controlling your joint weaken, and you may start to limp.
You will be referred to an orthopaedic surgeon and it is the responsibility of the specialist to determine the degree of osteoarthritis and your suitability for a total hip replacement. Your doctor will determine how much the disease has progressed. They may rotate, bend and extend your hips to check for pain. Both hips will be X-rayed to check if hip joint space has changed, and if you have developed bone spurs or other abnormalities.
In cases of osteoarthritis, the hip joint space will be narrowed and there will be extra bone pieces, known as osteophytes, projecting from the joint, suggesting the extra degree of arthritis. In rare cases, your doctor may request more advanced investigations such as an MRI.
What is Total Hip Replacement?
Total hip replacement is an operation performed at the end stage osteoarthritis of the hip, having failed all non-operative treatment.
Total hip replacement is one of the best orthopaedic operations, providing excellent pain relief and improving joint function. It has been practiced for well over 50 years and has had radical advances in technology over the years, to achieve even better results.
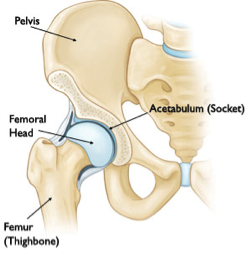
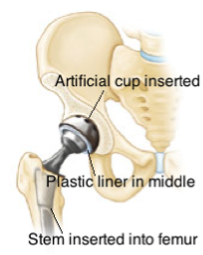
The diseased bone from the hip joint is cut and removed, then the socket is cored. Then a new prosthesis is either cemented (if you are older and the bone quality is not good) or tight fit into your bone with an intervening layer of plastic liner replacing the cartilage. Alternative materials to plastics are now used to improve the longevity of the hip replacement. These include ceramics bearing surfaces.
Normal Hip
Joint Diseased
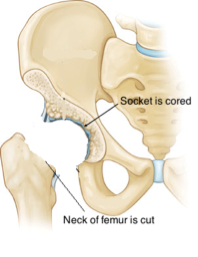
Hip joint removed
After surgery
Post-Operative Management:
It is normal to experience some pain following the operation, but adequate provisions will be made to reduce this considerably and ensure a comfort post operation. Mr Unni uses a special pain protocol during the operation to significantly reduce this pain.
Complications are rare but can occur. These include:
- Infection: Affecting 1-3% of patients depending on their pre-existing medical conditions. Appropriate antibiotics will be started and given for 24 hours to prevent infection.
- Deep vein thrombosis: Affecting 1-2% of patients and up to 10% if there are predisposing factors such as malignancy, previous deep vein thrombosis, blood diseases, smoking etc. Patients begin a course of medication for thinning your blood and given special stockings and calf or foot pumps as a preventive measure. Blood clots can very rarely migrate to your heart and lungs in extreme situations (pulmonary embolism) and may rarely cause death (0.02%)
- The artificial hip joint may dislocate: Mr Unni uses an approach that has an extremely low dislocation rate affecting 0.5% of patients.
- Neurovascular injury: This is extremely rare. However temporary weakness of the leg due to nerve bruising may uncommonly occur.
- Leg length discrepancy: A few millimetres of leg length inequality are likely to be noticed after a hip replacement, yet it’s not a common occurrence.
Other minor complications include fractures during the operation and inadequate fixation due to poor bone quality. These can be predicted before the operation and adequate measures are taken to prevent these complications occurring.
- General complications can be part of any surgery and they include urinary infection, anaemia (requiring blood transfusion), and chest infection.
Total hip replacement is a highly successful surgery and offers excellent pain relief with improvement of function.
What is anterior total hip replacement approach?
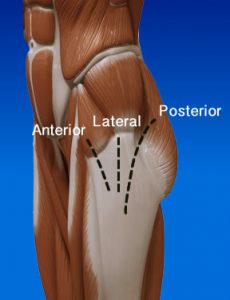 Hip replacement requires the surgeon to enter the hip joint via surgical incisions through the tissues. Traditionally these are done either through the lateral or the posterior route. Both of these approaches require the surgeon to cut muscles. This can elicit more pain in the immediate post-operative period. The anterior entry route for hip replacement was invented in late 1800’s and has sparingly been practiced. It has been more prevalent in Europe with good success. This approach spares all muscles from cutting and enters the hip joint between the muscles. It creates less pain post operatively and theoretically allows patients to walk on their new replaced hip sooner. No long-term benefits have been shown in the literature with this approach.
Hip replacement requires the surgeon to enter the hip joint via surgical incisions through the tissues. Traditionally these are done either through the lateral or the posterior route. Both of these approaches require the surgeon to cut muscles. This can elicit more pain in the immediate post-operative period. The anterior entry route for hip replacement was invented in late 1800’s and has sparingly been practiced. It has been more prevalent in Europe with good success. This approach spares all muscles from cutting and enters the hip joint between the muscles. It creates less pain post operatively and theoretically allows patients to walk on their new replaced hip sooner. No long-term benefits have been shown in the literature with this approach.
Mr. Unni has had training with this technique and uses it in suitable patients.
Before & After Anterior Approach
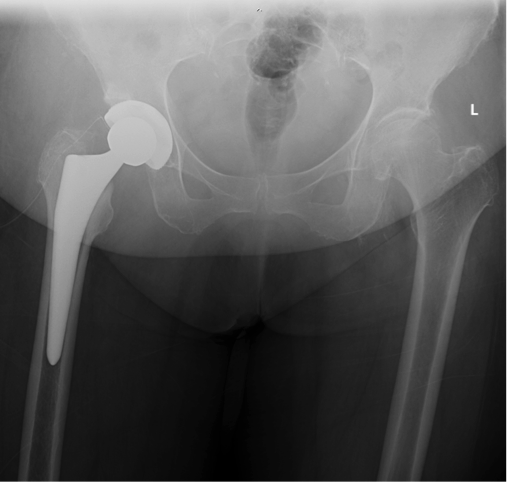
Pre-operative X-Ray:

Post-operative X-Ray: